Establishment and validation of a screening and risk predication model for rotator cuff tear and shoulder stiffness
Highlight box
Key findings
• The study identified eight pertinent risk factors: gender, dominant side, smoking, hypothyroidism, depression, hyperlipidemia, type III acromion, and partial tear VSports在线直播. Based on these factors, a clinical prediction model was developed.
What is known and what is new?
• Rotator cuff tear (RCT) with shoulder stiffness have a high association rate; however, the mechanism and possible risk factors are unclear.
• The study identified eight pertinent risk factors. Based on these factors, a clinical prediction model was developed VSports. The prediction model offers clinicians a simple and reliable tool for predicting the combination of RCT and shoulder stiffness.
What is the implication, and what should change now?
• This study has utilized routinely collected data to establish and validate a straightforward and dependable model for predicting the risk of RCT in conjunction with shoulder joint stiffness V体育官网. The model demonstrates strong differentiation and accuracy, offering valuable support for clinicians in making personalized clinical decisions based on individual patient risks.
Introduction
Rotator cuff tears (RCTs) are one of the most common causes of shoulder pain, muscle weakness and functional disabilities (1-4) VSports手机版. RCT directly lead to limited active motion of the shoulder, and a positive resistance test does not impede passive motion of the shoulder (2); however, patients with definite RCT and shoulder stiffness are often seen in clinical care, with a reported incidence of approximately 11 to 20 percent (5-9).
Inflammation and pain caused by RCT can lead to decline or loss of joint function, capsular contracture, muscle weakness, and ultimately joint stiffness (10-12). Diabetes mellitus, hypothyroidism, and cardiopulmonary and autoimmune diseases have been shown to be associated with shoulder stiffness (13-16) V体育安卓版. Understanding the pathogenesis and associated factors of RCT and shoulder stiffness is important since the management of such patients is clearly different from RCT alone, and it is often necessary to find a balance between joint immobilization and early functional exercise after rotator cuff repair, as joint immobilization promotes rotator cuff tendon healing and early mobilization to prevent recurrence of joint stiffness (17,18). Therefore, some doctors choose to undergo conservative treatment and rehabilitation to restore the normal range of motion of the shoulder joint before performing rotator cuff repair surgery. That being said, there is no conclusion on whether these patients have an increased risk of post-immobilization stiffness and its risk factors (19).
In conclusion, the risk factors for RCT combined with shoulder stiffness are still inconclusive (20). This study will collect the factors that may affect RCT and shoulder stiffness based on literature reports and clinical experience, screen out the relevant risk factors through statistical analysis, and establish and validate a simple model to predict the risk of RCT combined with shoulder stiffness. We present this article in accordance with the TRIPOD reporting checklist (available at https://aoj. amegroups. com/article/view/10 V体育ios版. 21037/aoj-25-16/rc).
Methods
"VSports最新版本" Clinical date collection
From December 2019 to June 2023, patients with RCT diagnosed through arthroscopic surgery at the Department of Joint and Sports Medicine of the First Affiliated Hospital of Dalian Medical University were selected. The inclusion and exclusion criteria are shown in Table 1 VSports最新版本.
V体育安卓版 - Table 1
| Case inclusion criteria |
| Patients with clinical diagnosis of RCT or RCT combined with stiffness |
| Case exclusion criteria |
| (I) Patients with missing case data and unable to complete through follow-up |
| (II) Other shoulder injuries such as osteoarthritis, periarticular fractures, SLAP, Bankart injuries, Hill-Sachs injuries, axillary nerve injuries, shoulder dislocations, and shoulder tumors |
| (III) Calcific tendonitis |
| (IV) History of previous shoulder surgery |
RCT, rotator cuff tear; SLAP, superior labrum, anterior and posterior.
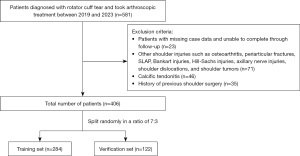
This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the ethics board of the First Affiliated Hospital of Dalian Medical University (No. PJ-KS-KY-2023-574) and informed consent was taken from all the patients. Of the 581 patients who met the inclusion criteria, 175 were excluded, and a total of 406 patients were included in the analysis, including 193 patients with RCT and 213 patients with RCT and shoulder stiffness. Using the R caret package (R soft-ware; version 4.2.0, Vienna, Austria), split randomly in a ratio of 7:3, patients (N=284) were assigned to the training set to construct a predictive model and the remaining patients (N=122) were assigned to the validation set to evaluate the model’s performance. The proportion of patients with RCT combined with shoulder stiffness in both the training set and the validation set was 52.5% (Figure 1).
Baseline data collection and diagnostic criteria
Demographic and clinical data was collected from the hospital electronic medical record (EMR) system. Data collected was based on literature as well as clinical experience (1,2,21-33), including: patient gender, age, smoking, marital status, duration, history of old trauma, dominant side, body mass index (BMI), hypertension, diabetes, cerebrovascular history, rheumatic immune disease, hypothyroidism, tumor, depression, hyperuricemia, hyperlipidemia, C-reactive protein (CRP) >8 mg/L, erythrocyte sedimentation rate (ESR) >20 mm/h, type III acromion, partial tear total 21 risk factors and range of motion of the shoulder (including forward flexion, external rotation, internal rotation), etc.
BMI was divided into underweight (BMI <18.5 kg/m2), normal (18.5≤ BMI <24 kg/m2), overweight (24≤ BMI <28 kg/m2), obesity (BMI ≥28 kg/m2); chronic trauma (defined as trauma to the affected shoulder for more than 3 months); rheumatoid immune diseases include ankylosing spondylitis, rheumatoid arthritis, psoriasis, etc.; diagnosis of depressed patients is based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), with three core symptoms: 1, depressed mood; 2, and loss of interest and pleasure; 3, loss of energy or tendency to get tired easily. If the patient meets two of the requirements, it is recommended that the patient go to a specialist for further diagnosis and treatment. Elevated CRP >8 mg/L and ESR >20 mm/h. Type III acromion was judged by supraspinatus outlet view and Bigliani acromion morphological typing; partial tear was confirmed by shoulder arthroscopy. According to the activity level of the patient during the preoperative physical examination in the EMR system, patients with shoulder flexion less than 100°, external rotation less than 30° and internal rotation of the thumb below L1 were included in the stiffness group according to the commonly used diagnostic criteria reported in the literature (21-23,34) and the remaining patients were included in the non-stiff group (Table 2).
V体育平台登录 - Table 2
| Variables | Non-stiffness (N=193) | Stiffness (N=213) | P value |
|---|---|---|---|
| Gender | 0.01 | ||
| Male | 113 (58.5) | 151 (70.9) | |
| Female | 80 (41.5) | 62 (29.1) | |
| Age (years) | 60.0 [54.0; 67.0] | 60.0 [53.0; 65.0] | 0.67 |
| Smoking | 0.14 | ||
| No | 164 (85.0) | 168 (78.9) | |
| Yes | 29 (15.0) | 45 (21.1) | |
| Marriage | 0.12 | ||
| Married | 183 (94.8) | 196 (92.0) | |
| Unmarried | 2 (1.0) | 1 (0.5) | |
| Divorced | 3 (1.6) | 12 (5.6) | |
| Widowed | 5 (2.6) | 4 (1.9) | |
| Duration (months) | 4.00 [2.00; 9.00] | 5.00 [3.00; 9.00] | 0.048 |
| History of old trauma | 0.61 | ||
| No | 128 (66.3) | 135 (63.4) | |
| Yes | 65 (33.7) | 78 (36.6) | |
| Dominant side | <0.001 | ||
| No | 65 (33.7) | 120 (56.3) | |
| Yes | 128 (66.3) | 93 (43.7) | |
| BMI (kg/m2) | 0.003 | ||
| <18.5 | 3 (1.6) | 5 (2.3) | |
| ≥18.5, <24 | 61 (31.6) | 98 (46.0) | |
| ≥24, <28 | 90 (46.6) | 89 (41.8) | |
| ≥28 | 39 (20.2) | 21 (9.9) | |
| Hypertension | 0.55 | ||
| No | 127 (65.8) | 133 (62.4) | |
| Yes | 66 (34.2) | 80 (37.6) | |
| Diabetes | 0.001 | ||
| No | 160 (82.9) | 145 (68.1) | |
| Yes | 33 (17.1) | 68 (31.9) | |
| Cerebrovascular history | 0.46 | ||
| No | 174 (90.2) | 186 (87.3) | |
| Yes | 19 (9.8) | 27 (12.7) | |
| Rheumatic autoimmune diseases | >0.99 | ||
| No | 184 (95.3) | 202 (94.8) | |
| Yes | 9 (4.7) | 11 (5.2) | |
| Hypothyroidism | 0.003 | ||
| No | 191 (99.0) | 197 (92.5) | |
| Yes | 2 (1.0) | 16 (7.5) | |
| Tumor history | 0.30 | ||
| No | 175 (90.7) | 185 (86.9) | |
| Yes | 18 (9.3) | 28 (13.1) | |
| Depression | <0.001 | ||
| No | 186 (96.4) | 173 (81.2) | |
| Yes | 7 (3.6) | 40 (18.8) | |
| Hyperuricemia | 0.98 | ||
| No | 167 (86.5) | 183 (85.9) | |
| Yes | 26 (13.5) | 30 (14.1) | |
| Hyperlipemia | <0.001 | ||
| No | 125 (64.8) | 78 (36.6) | |
| Yes | 68 (35.2) | 135 (63.4) | |
| CRP >8 mg/L | 0.20 | ||
| No | 186 (96.4) | 210 (98.6) | |
| Yes | 7 (3.6) | 3 (1.4) | |
| ESR >20 mm/h | 0.40 | ||
| No | 174 (90.2) | 198 (93.0) | |
| Yes | 19 (9.8) | 15 (7.0) | |
| Type III acromion | <0.001 | ||
| No | 130 (67.4) | 94 (44.1) | |
| Yes | 63 (32.6) | 119 (55.9) | |
| Partial tear | <0.001 | ||
| No | 162 (83.9) | 81 (38.0) | |
| Yes | 31 (16.1) | 132 (62.0) | |
Data are presented as n (%) or median [interquartile range]. BMI, body mass index; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate.
Data quality control
The clinical data collection and evaluation of the included patients were carried out in collaboration with two experienced shoulder arthroscopists. Laboratory tests and imaging examinations were all conducted at the First Affiliated Hospital of Dalian Medical University.
VSports app下载 - Statistical analysis
In this study, the data information of the included patients was anonymized before statistical analysis. Normally distributed continuous variables are represented as mean ± standard deviation, non-normally distributed variables are expressed as median (interquartile range), and categorical variables are expressed as number (percentage). The independent samples t-test was used for the difference test for normally distributed continuous variables, the nonparametric test was used for the difference test for non-normally distributed continuous variables, and the Chi-squared test or Fisher’s exact test was used for the difference analysis of categorical variables.
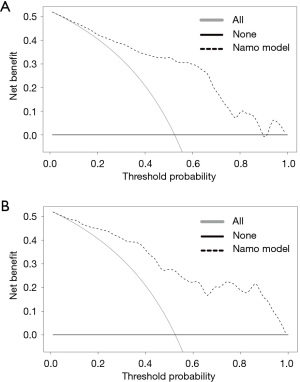
In this study, R soft-ware (version 4.2.0) was used for statistical analysis. Univariate logistic regression analysis was used to screen the risk factors associated with RCT and shoulder stiffness in the training set; the variables with a P value of <0.10 were regarded as significant risk factors for RCT combined with shoulder stiffness, and these factors were included in the multivariate logistic regression analysis to determine the clinical predictors of RCT combined with shoulder stiffness. Based on these clinical predictors, a clinical prediction model of RCT complicated with shoulder stiffness was developed through the RMS software package. The differentiation, calibration and clinical practicability of the model were verified through the training set and the validation set. The area under the receiver operating characteristic curve (AUROC) was plotted using the “pROC” package to evaluate the discriminant ability of the prediction model. The calibrate package evaluates the prediction accuracy of a predictive model by plotting a calibration curve. Decision curve analysis (DCA) was performed using the rmda software package, which can be used to quantify and compare the potential net benefits of the predictive model (35) to demonstrate the clinical effectiveness of the treatment strategy (35-37). All statistical tests were bilateral, and P<0.10 was statistically significant.
Results
Univariate and multivariate logistic regression analysis of the training set
A total of 21 suspected risk factors were included, and univariate logistic regression analysis showed that female sex, smoking, non-dominant side, diabetes mellitus, hypothyroidism, depression, hyperlipidemia, type III acromion, and partial tear were all risk factors for RCT and shoulder stiffness (P<0.10) (Table 3). Multivariate logistic regression analysis showed that gender [odds ratio (OR) =0.433, 95% confidence interval (CI): 0.204–0.894, P=0.03], smoking (OR =3.476, 95% CI: 1.473–8.632, P=0.006), dominant side (OR =0.492, 95% CI: 0.265–0.905, P=0.02), hypothyroidism (OR =5.518, 95% CI: 1.122–40.85, P=0.051), depression (OR =5.912, 95% CI: 2.039–20.08, P=0.002), hyperlipidemia (OR =2.953, 95% CI: 1.622–5.464, P<0.001), type III acromion (OR =3.148, 95% CI: 1.714–5.918, P<0.001), partial tear (OR = 7.707, 95% CI: 4.08–15.21, P<0.001) were related risk factors for RCT and stiffness (Table 4).
Table 3
| Characteristics | B | SE | OR | 95% CI | Z | P |
|---|---|---|---|---|---|---|
| Gender | −0.433 | 0.252 | 0.648 | 0.395–1.06 | −1.722 | 0.08 |
| Age (years) | 0.005 | 0.013 | 1.005 | 0.979–1.031 | 0.37 | 0.71 |
| Smoking | 0.568 | 0.310 | 1.765 | 0.97–3.287 | 1.834 | 0.07 |
| Marriage | ||||||
| Married | – | – | 1.000 | Reference | – | – |
| Unmarried | −0.77 | 1.231 | 0.463 | 0.021–4.893 | −0.625 | 0.53 |
| Divorced | 0.904 | 0.688 | 2.471 | 0.697–11.46 | 1.314 | 0.19 |
| Widowed | −0.076 | 0.718 | 0.926 | 0.215–3.993 | −0.106 | 0.92 |
| Duration | −0.009 | 0.012 | 0.991 | 0.968–1.014 | −0.745 | 0.46 |
| History of old trauma | 0.153 | 0.248 | 1.165 | 0.717–1.899 | 0.616 | 0.54 |
| Dominant side | −1.051 | 0.249 | 0.349 | 0.213–0.566 | −4.227 | <0.001 |
| BMI (kg/m2) | ||||||
| <18.5 | 1.000 | Reference | ||||
| ≥18.5, <24 | 0.115 | 0.934 | 1.122 | 0.143–7.04 | 0.123 | 0.90 |
| ≥24, <28 | −0.469 | 0.930 | 0.626 | 0.08–3.897 | −0.504 | 0.61 |
| ≥28 | −0.929 | 0.966 | 0.395 | 0.048–2.626 | −0.962 | 0.33 |
| Hypertension | 0.091 | 0.248 | 1.096 | 0.674–1.784 | 0.368 | 0.71 |
| Diabetes | 0.627 | 0.275 | 1.872 | 1.099–3.237 | 2.283 | 0.02 |
| Cerebrovascular history | 0.272 | 0.361 | 1.312 | 0.65–2.707 | 0.753 | 0.45 |
| Rheumatic autoimmune diseases | 0.479 | 0.638 | 1.614 | 0.476–6.281 | 0.75 | 0.45 |
| Hypothyroidism | 1.565 | 0.784 | 4.784 | 1.232–31.50 | 1.997 | 0.046 |
| Tumor history | 0.316 | 0.381 | 1.372 | 0.655–2.956 | 0.829 | 0.41 |
| Depression | 1.608 | 0.507 | 4.992 | 1.995–15.18 | 3.17 | 0.002 |
| Hyperuricemia | 0.002 | 0.342 | 1.002 | 0.512–1.97 | 0.005 | >0.99 |
| Hyperlipemia | 1.218 | 0.249 | 3.381 | 2.087–5.541 | 4.898 | <0.001 |
| CRP >8 mg/L | −15.695 | 727.699 | 0 | NA–2.594 | −0.022 | 0.98 |
| ESR >20 mm/h | −0.713 | 0.460 | 0.49 | 0.19–1.185 | −1.548 | 0.12 |
| Type III acromion | 1.183 | 0.249 | 3.264 | 2.013–5.357 | 4.743 | <0.001 |
| Partial tear | 1.949 | 0.283 | 7.025 | 4.09–12.45 | 6.885 | <0.001 |
BMI, body mass index; CI, confidence interval; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; NA, not available; OR, odds ratio; SE, standard error.
Table 4
| Characteristics | B | SE | OR | 95% CI | Z | P |
|---|---|---|---|---|---|---|
| Gender | −0.836 | 0.37582 | 0.433 | 0.204–0.894 | −2.225 | 0.03 |
| Smoking | 1.246 | 0.44928 | 3.476 | 1.473–8.632 | 2.773 | 0.006 |
| Dominant side | −0.709 | 0.31204 | 0.492 | 0.265–0.905 | −2.273 | 0.02 |
| Hypothyroidism | 1.708 | 0.876 | 5.518 | 1.122–40.85 | 1.95 | 0.051 |
| Depression | 1.777 | 0.57448 | 5.912 | 2.039–20.08 | 3.093 | 0.002 |
| Hyperlipemia | 1.083 | 0.30878 | 2.953 | 1.622–5.464 | 3.507 | <0.001 |
| Type III acromion | 1.147 | 0.31502 | 3.148 | 1.714–5.918 | 3.64 | <0.001 |
| Partial tear | 2.042 | 0.33456 | 7.707 | 4.08–15.21 | 6.104 | <0.001 |
CI, confidence interval; OR, odds ratio; SE, standard error.
V体育官网 - Predictive model building
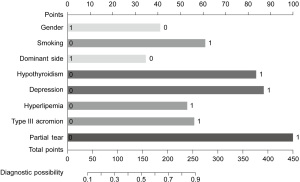
Multifactorial logistic regression analysis was used to screen the variables, from there 8 were selected. These included, gender, smoking, dominant side, hypothyroidism, depression, Hyperlipemia, type III acromion and partial tear. The model was visualised through construction of a nomogram (Figure 2). In this nomogram, each risk factor has its own corresponding score, and the total score is obtained by adding these scores. Then the probability of predicting the risk of having shoulder stiffness after RCT is the probability of “diagnostic possibility” corresponding to the “total points” in the figure.
Evaluation of predictive model performance
Based on the training set data, the differentiation analysis of the model was carried out by the AUROC, the accuracy analysis by the calibration curve, and the effectiveness analysis by the DCA. The AUROC was 0.856, 95% CI: 0.812–0.900 (Figure 3), the discrimination performance of the model was good, the calibration curve showed that the prediction probability comparison line was close to the ideal perfect agreement line (Figure 4), the prediction accuracy of the model was good, and the DCA showed that the effective range of the model was large (Figure 5).
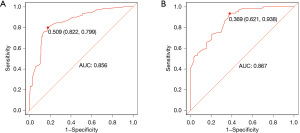
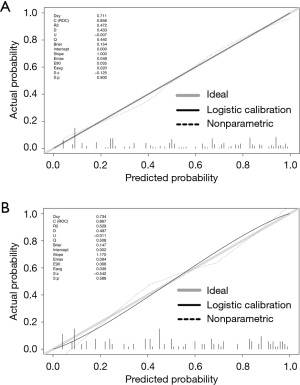
Predictive model validation (V体育2025版)
The validation set (n=122) data that did not participate in the model construction was used to validate the model internally, and to further evaluated the model performance. The results showed that the AUROC was 0.867, 95% CI: 0.807–0.928 (Figure 3), and the discrimination performance of the model was good, the calibration curve showed that the prediction probability comparison line was close to the ideal perfect agreement line (Figure 4), indicating that the model accuracy was good, and the DCA showed that the model had a large effective range (Figure 5).
"V体育ios版" Discussion
In this study, a simple risk prediction model for predicting the risk of RCT combined with shoulder joint stiffness was established and verified. The model incorporates routinely collected data, including gender, smoking, dominant side, hypothyroidism, depression, hyperlipemia, type III acromion, and partial tear. A total of 8 risk factors, in the training set and the validation set, respectively, showed good differentiation and calibration ability. In clinical practice, this model can easily score the risk of RCT combined with shoulder joint stiffness. In addition, by weighing the net benefits of individualized clinical decision-making, it will help doctors manage risk for patients.
Research shows that women are one of the predisposing factors for shoulder joint stiffness (24). Through research for this model, it was found that female gender is actually a significant risk factor for RCT combined with shoulder joint stiffness. However, a study of 303 patients with torn rotator cuff by Iwashita et al. showed that there were no significant differences in gender, disease duration, and diabetes between the stiff and non-stiff groups (22). In the afore mentioned study, the number of cases of RCT combined with shoulder joint stiffness was only 53, while in this study, a number of cases reached 213. The increase in sample size may affect the role of gender factors.
The results of this study also found that smoking is a significant risk factor for RCT combined with shoulder joint stiffness. This finding is consistent with the research of Iwashita et al. (21,22). As a predisposing factor for a variety of diseases, smoking plays a negative role in a variety of diseases of the skeletal muscle system. At present, the main hypotheses for its role in shoulder joint stiffness are: causing blood vessels to constrict, leading to tissue hypoxia, and a decrease in the patient’s pain threshold (25).
In this study, it was found that the probability of RCT combined with shoulder joint stiffness on the dominant side was significantly lower than that on the opposite side. In this study, it is believed that unless it is clearly diagnosed and bracing is required, the dominant shoulder joint is rarely strictly restricted in activity. From another point of view, it can be considered that the dominant shoulder joint has undergone rehabilitation exercises, thereby reducing the incidence of shoulder stiffness. However, it was also found that the number of anchors used to repair the rotator cuff during surgery in the non-stiff group increased significantly, indicating that there were more large or huge RCT in the non-stiff group. Therefore, the dominant side is a protective factor for shoulder joint stiffness, but the dominant side may be further aggravated by RCT because it cannot restrict activities well, which eventually leads to huge RCT and osteoarthritis. Therefore, clinicians should pay attention to shoulder pain, make a clear diagnosis early, and not blindly treat and exercise.
Through an analysis and comparison of the surgical approaches used in the two patient groups, we observed that in cases of RCT combined with shoulder joint stiffness, it is essential to first perform capsular release and release of the glenohumeral ligaments to alleviate stiffness. Only after restoring joint mobility can rotator cuff repair be effectively carried out. In patients with RCT alone, particularly those with massive or irreparable tears, additional procedures such as tendon transfer or superior capsular reconstruction may be necessary to achieve optimal outcomes.
At present, more studies believe that hypothyroidism, diabetes, depression, and hyperlipemia are high-risk factors for frozen shoulder (26-33). The pathogenesis of frozen shoulder is not yet clear. Synovial inflammation, joint capsule fibrosis, and cartilage formation are considered to play a key role and may be related to neurological, immune, or endocrine disorders (34). Yamaura et al. believe that shoulder joint stiffness associated with rotator cuff may have the same pathology as primary frozen shoulder (2).
Through this study, hypothyroidism, depression, and hyperlipemia are shown as risk factors for RCT combined with shoulder joint stiffness, while diabetes is not a significant risk factor. Therefore, we believe that there is a difference in the pathogenesis of RCT combined with shoulder joint stiffness and frozen shoulder.
The relationship between acromion morphology and RCT type and shoulder joint stiffness is rarely reported in the literature. This study shows that there is a significant correlation between type III acromion and RCT combined with shoulder joint stiffness. It suggests that type III acromion is more likely to induce shoulder joint impact syndrome and rotator cuff injury, which causes bursitis inflammation and pain, and shoulder joint mobility will be significantly limited, which will lead to shoulder joint stiffness as the disease progresses. Study by Iwashita et al. has shown that the incidence of shoulder joint stiffness in patients with partial RCT is significantly higher than that of patients with full RCT (22). Ueda et al. pointed out that severe frozen shoulders rarely have full-layer RCT (23). In this study, it found that partial RCT can cause inflammation and pain, resulting in restricted shoulder joint movement and stiffness. However, patients with RCT who do not have stiff shoulder joints may eventually experience further aggravated RCT, or even huge tears. It is known that huge RCT rarely merge with shoulder joint stiffness. This research study shows that there are very few patients with shoulder joint stiffness combined with large RCT and huge tears. Patients with torn rotator cuff combined with stiff shoulder joints use a small number of anchors during surgery. Because of this the quality of the remaining rotator cuff in patients with partial torn rotator cuff combined with stiff shoulder joints is acceptable, and the probability of changing to a full-layer tear during surgery is low.
Although partial tears are sometimes difficult to diagnose, given the significant correlation between partial tears and RCT combined with shoulder joint stiffness, this model still includes partial tears as a factor. Therefore, in the diagnosis and treatment, the shoulder joint magnetic resonance imaging should be carefully analysed to clarify the degree of RCT and refine the diagnosis and treatment.
Trauma can cause bleeding and unwillingness to move the shoulder joint (1), and the physiological movement of the shoulder joint and scapula can also be restricted, resulting in stiffness of the shoulder joint. There is no general consensus on the cause of shoulder joint stiffness after trauma. The causes of shoulder joint stiffness after trauma are dynamic and very complex (21). Seo et al. pointed out that traumatic RCT have a 42.9% incidence of shoulder joint stiffness; while non-traumatic RCT only 22.8% of stiffness occurs (1). This research study shows that the history of trauma to the shoulder joint 3 months ago is not a risk factor for RCT combined with shoulder joint stiffness. Through research it was found that the severity of shoulder injury and the time from the injury to the appearance of stiffness are difficult to define, but that the standardized diagnosis, treatment and rehabilitation after shoulder injury are very critical.
In conclusion, a significant correlation exists between gender, smoking habits, dominant side of the body, hypothyroidism, depression, hyperlipemia, type III acromion morphology, partial tear and RCT combined with shoulder joint stiffness.
In the future, this predictive model could be integrated into the hospital information system. Once a patient provides the necessary clinical information during a visit, the system can automatically calculate the risk score and estimate the corresponding probability. This would enable physicians to efficiently identify patients at risk for RCT with shoulder stiffness and offer appropriate guidance and treatment.
This study has certain limitations. Firstly, the sample size is limited and there was heterogeneity among studies in terms of the outcome measures evaluated. Secondly, this study is a retrospective analysis, all the materials are from the EMR data. Due to recording errors, the obtained clinical data may be biased from the actual situation. Thirdly, in the process of applying this modeling method, there may be a phenomenon of confounding bias. Finally, the current conclusions still need to be confirmed through incorporating a large sample of forward-looking, multi-centre research in the future.
Conclusions
In summary, this study has utilized routinely collected data to establish and validate a straightforward and dependable model for predicting the risk of RCT in conjunction with shoulder joint stiffness. The model demonstrates strong differentiation and accuracy, offering valuable support for clinicians in making personalized clinical decisions based on individual patient risks.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the TRIPOD reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-25-16/rc
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-25-16/dss
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-25-16/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-25-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the ethics board of the First Affiliated Hospital of Dalian Medical University (No. PJ-KS-KY-2023-574) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Seo SS, Choi JS, An KC, et al. The factors affecting stiffness occurring with rotator cuff tear. J Shoulder Elbow Surg 2012;21:304-9. [Crossref] [PubMed]
- Yamaura K, Mifune Y, Inui A, et al. Sex Is Associated with the Success or Failure of Manipulation Alone for Joint Stiffness Associated with Rotator Cuff Repair. J Clin Med 2022;11:7192. [V体育ios版 - Crossref] [PubMed]
- Cerciello S, Mocini F, Proietti L, et al. Critical Shoulder Angle in Patients With Cuff Tears. Sports Med Arthrosc Rev 2024;32:38-45. ["VSports注册入口" Crossref] [PubMed]
- Liu A, Zhang B, Lai T, et al. Comparison of functional outcomes following early and delayed arthroscopic repair for traumatic and non-traumatic rotator cuff injuries. J Orthop Surg Res 2024;19:368. [Crossref] [PubMed]
- Chen Y, Chen S, Qiao Y, et al. A Long Preoperative Duration of Symptoms Is Associated With Worse Functional Outcomes After 1-Stage Arthroscopic Treatment of Rotator Cuff Tears With Shoulder Stiffness. Am J Sports Med 2017;45:2336-44. [Crossref] [PubMed]
- Ho WP, Huang CH, Chiu CC, et al. One-stage arthroscopic repair of rotator cuff tears with shoulder stiffness. Arthroscopy 2013;29:1283-91. ["VSports注册入口" Crossref] [PubMed]
- Hsu SL, Ko JY, Chen SH, et al. Surgical results in rotator cuff tears with shoulder stiffness. J Formos Med Assoc 2007;106:452-61. [Crossref] [PubMed]
- Kim IB, Jung DW. A Rotator Cuff Tear Concomitant With Shoulder Stiffness Is Associated With a Lower Retear Rate After 1-Stage Arthroscopic Surgery. Am J Sports Med 2018;46:1909-18. [Crossref] [PubMed]
- Yoon JY, Han H, Shin MY, et al. What is the most predictive magnetic resonance imaging finding of rotator cuff tear concomitant with shoulder stiffness? JSES Int 2023;7:756-62. [Crossref (VSports)] [PubMed]
- Chung SW, Huong CB, Kim SH, et al. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy 2013;29:290-300. [V体育安卓版 - Crossref] [PubMed]
- Cho NS, Rhee YG. Functional outcome of arthroscopic repair with concomitant manipulation in rotator cuff tears with stiff shoulder. Am J Sports Med 2008;36:1323-9. [Crossref] [PubMed]
- Kim YS, Lee HJ, Park I, et al. Are delayed operations effective for patients with rotator cuff tears and concomitant stiffness? An analysis of immediate versus delayed surgery on outcomes. Arthroscopy 2015;31:197-204. [Crossref] [PubMed]
- Pietrzak M. Adhesive capsulitis: An age related symptom of metabolic syndrome and chronic low-grade inflammation?. Med Hypotheses 2016;88:12-17. ["V体育ios版" Crossref] [PubMed]
- Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J 2016;6:26-34. [Crossref] [PubMed]
- Oliva F, Osti L, Padulo J, et al. Epidemiology of the rotator cuff tears: a new incidence related to thyroid disease. Muscles Ligaments Tendons J 2014;4:309-14.
- Schiefer M, Teixeira PFS, Fontenelle C, et al. Prevalence of hypothyroidism in patients with frozen shoulder. J Shoulder Elbow Surg 2017;26:49-55. [Crossref] [PubMed]
- Sabzevari S, Kachooei AR, Giugale J, et al. One-stage surgical treatment for concomitant rotator cuff tears with shoulder stiffness has comparable results with isolated rotator cuff tears: a systematic review. J Shoulder Elbow Surg 2017;26:e252-8. [V体育官网 - Crossref] [PubMed]
- Huberty DP, Schoolfield JD, Brady PC, et al. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy 2009;25:880-90. [Crossref] [PubMed]
- Yao L, Li Y, Li T, et al. One-stage rotator cuff repair in stiff shoulders shows comparable range of motion, clinical outcome and retear rates to non-stiff shoulders: a systematic review. J Orthop Surg Res 2023;18:613. [Crossref] [PubMed]
- Ko JY, Wang FS. Rotator cuff lesions with shoulder stiffness: updated pathomechanisms and management. Chang Gung Med J 2011;34:331-40.
- Itoi E, Arce G, Bain GI, et al. Shoulder Stiffness: Current Concepts and Concerns. Arthroscopy 2016;32:1402-14. [VSports手机版 - Crossref] [PubMed]
- Iwashita S, Hashiguchi H, Yoneda M, et al. Characteristics of the Patients with Rotator Cuff Tears with Stiffness. Arthroscopy 2017;33:e167.
- Ueda Y, Sugaya H, Takahashi N, et al. Rotator Cuff Lesions in Patients with Frozen Shoulder: An Analysis of 376 Stiff Shoulders. Journal of Shoulder and Elbow Surgery 2014;23:e320.
- White D, Choi H, Peloquin C, et al. Secular trend of adhesive capsulitis. Arthritis Care Res (Hoboken) 2011;63:1571-5. ["V体育2025版" Crossref] [PubMed]
- Hill CL, Gill TK, Shanahan EM, et al. Prevalence and correlates of shoulder pain and stiffness in a population-based study: the North West Adelaide Health Study. Int J Rheum Dis 2010;13:215-22. [Crossref] [PubMed]
- Balci N, Balci MK, Tüzüner S. Shoulder adhesive capsulitis and shoulder range of motion in type II diabetes mellitus: association with diabetic complications. J Diabetes Complications 1999;13:135-40. [Crossref] [PubMed]
- Bannwarth B. Drug-induced musculoskeletal disorders. Drug Saf 2007;30:27-46. ["VSports注册入口" Crossref] [PubMed]
- Bowman CA, Jeffcoate WJ, Pattrick M, et al. Bilateral adhesive capsulitis, oligoarthritis and proximal myopathy as presentation of hypothyroidism. Br J Rheumatol 1988;27:62-4. [V体育官网入口 - Crossref] [PubMed]
- Bridgman JF. Periarthritis of the shoulder and diabetes mellitus. Ann Rheum Dis 1972;31:69-71. [Crossref] [PubMed]
- Huang YP, Fann CY, Chiu YH, et al. Association of diabetes mellitus with the risk of developing adhesive capsulitis of the shoulder: a longitudinal population-based followup study. Arthritis Care Res (Hoboken) 2013;65:1197-202. ["VSports手机版" Crossref] [PubMed]
- Tighe CB, Oakley WS Jr. The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. South Med J 2008;101:591-5. [Crossref] [PubMed]
- Debeer P, Franssens F, Roosen I, et al. Frozen shoulder and the Big Five personality traits. J Shoulder Elbow Surg 2014;23:221-6. [Crossref] [PubMed]
- Armstrong A. Diagnosis and clinical assessment of a stiff shoulder. Shoulder Elbow 2015;7:128-34. [Crossref (V体育安卓版)] [PubMed]
- Tan Z, Hendy BA, Zmistowski B, et al. Glenohumeral synovitis score predicts early shoulder stiffness following arthroscopic rotator cuff repair. J Orthop 2020;22:17-21. ["V体育安卓版" Crossref] [PubMed]
- Kerr KF, Brown MD, Zhu K, et al. Assessing the Clinical Impact of Risk Prediction Models With Decision Curves: Guidance for Correct Interpretation and Appropriate Use. J Clin Oncol 2016;34:2534-40. [Crossref] [PubMed]
- Vickers AJ, Cronin AM, Elkin EB, et al. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak 2008;8:53. [Crossref] [PubMed]
- Van Calster B, Wynants L, Verbeek JFM, et al. Reporting and Interpreting Decision Curve Analysis: A Guide for Investigators. Eur Urol 2018;74:796-804. [Crossref] [PubMed]
Cite this article as: Sun X, Qi J, Zhang L, Hooblal AP, Wagner T, Wong ZY, Wang F, Zhang W, Tian K. Establishment and validation of a screening and risk predication model for rotator cuff tear and shoulder stiffness. Ann Joint 2025;10:24.


 "V体育官网"
"V体育官网"