Detriment of subchondral plate violation in antegrade osteochondral procedures—lessons and future direction
Introduction
The come and go of microfracture (V体育平台登录)
Background
The microfracture procedure was first described in 1994 by Dr. Steadman (1). It involves creating multiple small perforations in the subchondral bone plate, with the aim of promoting chondral resurfacing by removing the calcified layer of the lesion. The calcified layer is a barrier to prevent the migration of the bone marrow and blood in the lesion that causes fibrocartilage formation. Therefore, Steadman believed that its removal leveraged the body’s natural healing processes to fill the lesion with fibrocartilage VSports最新版本.
Early literature by Dr. Steadman demonstrated microfracture as a relatively efficacious surgical option for the treatment of osteochondral defects in numerous anatomic locations (2-5). For example, in a case series of 81 patients with isolated chondral lesions of the knee treated with microfracture, the authors found significantly improved patient reported outcome scores (4). Similarly, in another study focusing on cartilage injury in the shoulder, they found improved postoperative American Shoulder and Elbow Surgeons (ASES) scores following microfracture in 31 shoulders with smaller chondral lesions V体育平台登录. In this study, there was a negative correlation between the size of the lesion and ASES improvement and an overall failure rate of 19% requiring another surgical procedure (5).
The microfracture procedure has declined in popularity due to its limited indications and poor long-term outcomes. In 2010, Miller et al. analyzed clinical outcomes following microfracture for chondral defects of the knee. While the Lysholm score improved postoperatively, it steadily declined after two years (6). Additionally, Kreuz et al. found that patients over 40 years old had worse outcomes, potentially secondary to reduced regenerative capacity of the host tissue (2). While good results were found in young active patients with small cartilage defects, these results began to deteriorate at 18 months postoperatively. Furthermore, a systematic review including 15 studies found that beyond five years postoperatively, treatment failure and osteoarthritis were expected regardless of lesion size (7). Overall, the literature highlights concerns about the limitations of microfracture, such as variability in cartilage regeneration response, pain relief, and long-term outcomes (2,8,9) VSports注册入口.
Rationale and knowledge gap
The currently accepted treatment options for full-thickness osteochondral injuries include microfracture, drilling, autologous chondrocyte implantation (ACI), subchondroplasty, mosaicplasty, osteochondral allograft/autograft transplantation (OAT), or acellular implants V体育官网入口. Although microfracture has declined in popularity, there is debate that some of the aforementioned treatment modalities still incorporate one of Steadman’s foundational principles—the removal of the calcified cartilage layer to facilitate the formation of hyaline-like cartilage.
A 2022 meta-analysis of level 1 studies with a minimum follow-up of 5 years demonstrated superiority of ACI and OAT as compared to microfracture (10). A 2023 network meta-analysis on randomized clinical trials also showed the superiority of osteochondral transfer or transplantation compared to either microfracture or ACI (11). For patients with persistent bone marrow lesions secondary to mild to moderate knee osteoarthritis, subchondroplasty has been demonstrated to produce good outcomes (12). Given the multitude of treatment options available for osteochondral injuries, considerable research has focused on determining the most effective interventions based on specific lesion characteristics. For instance, Bekkers et al. conducted a systematic review analyzing parameters to guide treatment selection in articular cartilage repair of the knee (13). Their analysis revealed that larger lesions (>2 VSports在线直播. 5 cm2) showed better results following treatment with sophisticated techniques, such as ACI or OAT, compared to microfracture. The decline in the utility of microfracture is in part driven by the poor long-term performance of antegrade microfracture procedures, and in part by parallel translational evidence of rapid subchondral bone degradation following subchondral venting (14). With advent of directional drilling devices, a preference has emerged for antegrade drilling (15).
Objective
The objective of this review is to critically examine the current literature on subchondral plate violation in antegrade osteochondral procedures. We aim to highlight the detrimental effects of subchondral disruption on joint outcomes, synthesize emerging evidence on the biological and mechanical consequences, and identify future directions for optimizing osteochondral repair strategies while preserving subchondral integrity V体育2025版.
Antegrade procedures and risks
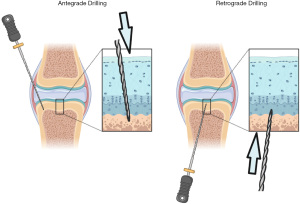
Antegrade procedures refer to approaching the cartilage defect from within the joint cavity (Figure 1). As an example, one treatment option for osteochondritis dissecans of the knee is arthroscopic antegrade drilling, which involves drilling holes orthogonal to the articular cartilage until reaching subchondral bone (16) VSports.
It has been proposed that microfracture, antegrade drilling, and other marrow-stimulating antegrade techniques allow bone marrow to escape from subchondral bone and actively contribute to the formation of fibrocartilage to fill cartilage defects (17). The potential for marrow products on healing has been demonstrated by previous studies highlighting the potential for use of marrow-derived stem cells from bone marrow aspirate in the repair of cartilage injuries (18,19). However, there is limited evidence supporting the migration of marrow progenitors out of subchondral bone and consequential formation of functional cartilage after microfracture or antegrade drilling alone (20) VSports app下载. Conversely, it is thought that the articular pressure generated from range of motion and weight bearing causes synovial fluid to infiltrate into bone, rather than permit marrow elements from emerging and contributing substantially to formation of neocartilage (21).
Previous studies have suggested that antegrade repair procedures for cartilage defects, such as microfracture, better facilitate the repair of defects compared to no treatment (14). However, these techniques inherently cause damage to subchondral structures, and studies have identified that there are detrimental effects of violating the subchondral plate (14,22,23). Breinan et al. conducted a study in a canine model showing that 15 weeks after microfracture for cartilage defects, the subchondral bone plate that was violated by the procedure had only 36% of this layer remaining intact, compared to 89% in the control group that did not receive microfracture (22). This lack of intact subchondral bone plate may predispose to long-term joint pathology such as osteoarthritis, given the important role of the subchondral bone plate in supporting and protecting cartilage during joint loading (24). A study by Beck et al. showed that microfracture in a sheep model was superior to no treatment of articular cartilage defects, but overall, this technique produced minimal cartilage fill, poor quality repair tissue, and induced severe pathology of the subchondral bone, which brings to question the durability of the repair (14). Microfracture was shown to promote the formation of subchondral bone cysts that, upon closer analysis, exhibited inflammatory and mechanical changes that resulted in increased bone volume, trabecular thickening, and decreased complexity of trabecular pattern beyond the region of the cartilage defect (14). Similarly, Orth et al. investigated subchondral drilling in a sheep model and found that drilling induced the formation of osteophytes along with subchondral cysts (23). Additionally, six months postoperatively, bone volume and mineral density of the subchondral bone below the cartilage defect were significantly decreased. Therefore, not only is there limited evidence that antegrade procedures release bone marrow progenitors into the joint, but there is converging evidence that microfracture triggers a cascade of processes that cause further irreversible pathology in the subchondral zone where sensory free nerve endings reside (25). In defects that were not affected by cysts, fibrocartilage fill is encountered; however, in defects affected by subchondral cysts, the region is instead filled by poorly differentiated matrix and exhibits surface depressions, compromising the cartilage repair (14).
"V体育平台登录" Drilling vs. microfracture
"VSports在线直播" What is the difference?
Microfracture is a bone marrow stimulation technique developed to promote the repair of damaged articular surfaces. First described by Steadman et al. in 1994, the procedure involves the use of an arthroscopic awl to create multiple small perforations in the subchondral bone (1). This environment is meant to trigger an osteochondral healing response and promote cartilage regeneration (3). This process reliably triggers the differentiation and formation of de novo fibrocartilage, which may contain varying amounts of type II collagen and ultimately heals the articular defect (26).
An important point made by Dr. Steadman in the microfracture process is not to create holes, but rather to create a series of radially oriented subchondral fracture patterns that diverge from awl strike points. As such, awl strikes are to be performed in a swift and sudden manner but not to a significant depth. The holes created by the microfracture procedure must be separated enough to preserve the integrity of the subchondral bone, separated by roughly 3 to 4 mm and impacted to a depth of 4 mm (27). Drilling, unlike microfracture, involves creating holes in themselves and does not create microscopic fracture patterns. Drilling thus solely vents the subchondral bone. This technique uses small drill bits or K-wires to create holes approximately 6 mm deep, forming direct channels to expose the joint environment to the subchondral marrow elements (27,28).
What is the biological difference?
Fundamentally, both microfracture and drilling create venting of the subchondral plate, even though intentions differ in their purported effect on osteochondral response. In an animal study investigating bone marrow stimulation techniques in an adult rabbit model, there were differences noted between the resultant subchondral bone changes after microfracture vs. drilling. After microfracture, fractures and impaction of the bone were observed, but the channels created by the awl were eventually obstructed by compressed bone (28). Following drilling, the resultant channels remained open with a direct connection to the subchondral environment (28). This study also noted a larger hematoma after drilling compared to microfracture which suggests a greater release of blood and subchondral nutrients. Furthermore, a cadaveric study found that drilling significantly reduced overall bone destruction as compared to microfracture due to the subsequent compressive impact caused by microfracture (29). According to some studies, microfracture is considered a safer procedure for minimizing bone injury, as there were concerns that drilling could cause thermal necrosis of the bone due to the heat generated during the process (27,30,31). Chen et al. challenged this idea, as they found that drilling did not result in increased osteocyte death from heat necrosis, instead observing greater osteocyte death and more empty lacunae caused by the crushing forces and compression associated with the microfracture procedure (28). In both procedures, however, concerns still remain about the long-term outcomes following venting of the subchondral plate.
Conclusions
Retrograde procedures—a possible way of the future?
Retrograde drilling may be a solution to mitigate the pitfalls of antegrade procedures. It involves drilling from beneath the osteochondral lesion to encourage revascularization of the subchondral bone, promoting new bone formation while preserving the cartilage layer and/or the subchondral plate (Figure 1). Current applications of retrograde techniques include subchondral fracture fixation and drilling for avascular necrosis. Marrow stimulation in this way should, with or without chondroplasty or chondral surface repair, trigger a reparative process in the osteochondral organ while avoiding the pitfalls of subchondral plate venting. A study by Minas et al. compared the failure rate of ACI after previous treatment with marrow-stimulating techniques that required subchondral bone violation (32). Defects that had prior treatment involving the subchondral bone had a clinical failure rate 3 times higher than primary defects. While this evidence does not directly link subchondral plate integrity to clinical failure, it is nevertheless cause for concern in patients with radiographic findings of subchondral disease.
The critical question thus still remains unanswered: is preservation of the subchondral plate essential in maintaining durability of cartilage repair? The answer may depend on the balance between achieving sufficient bone marrow stimulation for healing while maintaining the structural integrity of the subchondral plate to support long-term joint function and prevent further degeneration. Data is critically lacking in understanding this process. Retrograde drilling with subchondral plate preservation for cartilage repair may be an answer but is pending clinical comparative studies to demonstrate its efficacy prior to widespread adoption. Emerging cartilage repair strategies—including cell reprogramming, advanced biologic scaffolds, nano-gradient engineering, and copper-free click chemistry—hold promise for future integration into retrograde procedures as these technologies continue to evolve.
"VSports最新版本" Acknowledgments
The authors would like to thank the University of Pennsylvania Orthopaedics 2024 Cartilage Repair Symposium and Edward DiCarlo MD for lessons and inspiration for this topic.
V体育ios版 - Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Current Concepts and Techniques in Soft Tissue Repair and Joint Preservation”. The article has undergone external peer review.
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-69/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-69/coif). The series “Current Concepts and Techniques in Soft Tissue Repair and Joint Preservation” was commissioned by the editorial office without any funding or sponsorship. T.C. served as the unpaid Guest Editor of the series. T.C. reports that he serves as a member of the AOSSM Research Committee, receives support for attending meetings and/or travel from AOSSM Hip Think Tank, and has ownership and board positions at Sustain Surgical Inc. and Kondral Tech Inc. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rodrigo JJ, Steadman JR, Silliman JF, et al. Improvement of full-thickness chondral defect healing in the human knee after debridement and microfracture using continuous passive motion. Am J Knee Surg 1994;7:109-16.
- Kreuz PC, Steinwachs MR, Erggelet C, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage 2006;14:1119-25. [Crossref] [PubMed]
- Steadman JR, Rodkey WG, Singleton SB, et al. Microfracture technique for full-thickness chondral defects: Technique and clinical results. Oper Tech Orthop 1997;7:300-4.
- Miller BS, Steadman JR, Briggs KK, et al. Patient satisfaction and outcome after microfracture of the degenerative knee. J Knee Surg 2004;17:13-7. ["VSports" Crossref] [PubMed]
- Millett PJ, Huffard BH, Horan MP, et al. Outcomes of full-thickness articular cartilage injuries of the shoulder treated with microfracture. Arthroscopy 2009;25:856-63. [Crossref] [PubMed]
- Miller BS, Briggs KK, Downie B, et al. Clinical Outcomes following the Microfracture Procedure for Chondral Defects of the Knee: A Longitudinal Data Analysis. Cartilage 2010;1:108-12. [Crossref] [PubMed]
- Goyal D, Keyhani S, Lee EH, et al. Evidence-based status of microfracture technique: a systematic review of level I and II studies. Arthroscopy 2013;29:1579-88. [Crossref] [PubMed]
- Weber AE, Locker PH, Mayer EN, et al. Clinical Outcomes After Microfracture of the Knee: Midterm Follow-up. Orthop J Sports Med 2018;6:2325967117753572. ["V体育安卓版" Crossref] [PubMed]
- Kraeutler MJ, Aliberti GM, Scillia AJ, et al. Microfracture versus drilling of articular cartilage defects: a systematic review of the basic science evidence. Orthop J Sports Med 2020;8:2325967120945313. [Crossref] [PubMed]
- Angele P, Zellner J, Schröter S, et al. Biological Reconstruction of Localized Full-Thickness Cartilage Defects of the Knee: A Systematic Review of Level 1 Studies with a Minimum Follow-Up of 5 Years. Cartilage 2022;13:5-18. [Crossref] [PubMed]
- Muthu S, Viswanathan VK, Chellamuthu G, et al. Clinical effectiveness of various treatments for cartilage defects compared with microfracture: a network meta-analysis of randomized controlled trials. Journal of Cartilage & Joint Preservation 2024;4:100163.
- Di Matteo B, Anzillotti G, Conte P, et al. Subchondroplasty® (SCP) Provides Resolution of Symptoms and Functional Improvements in Mild-to-Moderate Knee Osteoarthritis with Persistent Bone Marrow Lesions: 12-Month Follow-Up Results from a Multicentric Open-Label Prospective Clinical Trial. Cartilage 2025;16:181-9. [VSports app下载 - Crossref] [PubMed]
- Bekkers JE, Inklaar M, Saris DB. Treatment selection in articular cartilage lesions of the knee: a systematic review. Am J Sports Med 2009;37:148S-55S. [Crossref] [PubMed]
- Beck A, Murphy DJ, Carey-Smith R, et al. Treatment of Articular Cartilage Defects With Microfracture and Autologous Matrix-Induced Chondrogenesis Leads to Extensive Subchondral Bone Cyst Formation in a Sheep Model. Am J Sports Med 2016;44:2629-43. ["VSports app下载" Crossref] [PubMed]
- Organizational website. [Accessed on October 15th, 2024]. Available online: https://www.stryker.com/us/en/sports-medicine/products/phoenix-microfracture-system.html
- Tudisco C, Bernardi G, Manisera MT, et al. An update on osteochondritis dissecans of the knee. Orthop Rev (Pavia) 2022;14:38829. [Crossref] [PubMed]
- Douleh D, Frank RM. Marrow stimulation: Microfracture, drilling, and abrasion. Oper Techn Sport Med 2018;26:170-4.
- Saw KY, Hussin P, Loke SC, et al. Articular cartilage regeneration with autologous marrow aspirate and hyaluronic Acid: an experimental study in a goat model. Arthroscopy 2009;25:1391-400. [VSports最新版本 - Crossref] [PubMed]
- Fortier LA, Potter HG, Rickey EJ, et al. Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J Bone Joint Surg Am 2010;92:1927-37. [Crossref] [PubMed]
- Cavinatto L, Hinckel BB, Tomlinson RE, et al. The Role of Bone Marrow Aspirate Concentrate for the Treatment of Focal Chondral Lesions of the Knee: A Systematic Review and Critical Analysis of Animal and Clinical Studies. Arthroscopy 2019;35:1860-77. ["V体育官网" Crossref] [PubMed]
- Cox LG, Lagemaat MW, van Donkelaar CC, et al. The role of pressurized fluid in subchondral bone cyst growth. Bone 2011;49:762-8. [Crossref] [PubMed]
- Breinan HA, Martin SD, Hsu HP, et al. Healing of canine articular cartilage defects treated with microfracture, a type-II collagen matrix, or cultured autologous chondrocytes. J Orthop Res 2000;18:781-9. [Crossref] [PubMed]
- Orth P, Goebel L, Wolfram U, et al. Effect of subchondral drilling on the microarchitecture of subchondral bone: analysis in a large animal model at 6 months. Am J Sports Med 2012;40:828-36. [Crossref] [PubMed]
- Stewart HL, Kawcak CE. The Importance of Subchondral Bone in the Pathophysiology of Osteoarthritis. Front Vet Sci 2018;5:178. [V体育安卓版 - Crossref] [PubMed]
- Morgan M, Nazemian V, Harrington K, et al. Mini review: The role of sensory innervation to subchondral bone in osteoarthritis pain. Front Endocrinol (Lausanne) 2022;13:1047943. [Crossref] [PubMed]
- Mithoefer K, Williams RJ 3rd, Warren RF, et al. The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg Am 2005;87:1911-20. [Crossref] [PubMed]
- Ozmeriç A, Alemdaroğlu KB, Aydoğan NH. Treatment for cartilage injuries of the knee with a new treatment algorithm. World J Orthop 2014;5:677-84. [Crossref] [PubMed]
- Chen H, Sun J, Hoemann CD, et al. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res 2009;27:1432-8. [Crossref] [PubMed]
- Meyer LE, Danilkowicz RM, Hinton ZW, et al. Microdrilling Resulted in Less Subchondral Bone Destruction Than a Traditional Microfracture Awl for Articular Cartilage Defect Bone Marrow Stimulation. Arthrosc Sports Med Rehabil 2023;5:100786. [Crossref] [PubMed]
- Jarecki J, Waśko MK, Widuchowski W, et al. Knee Cartilage Lesion Management-Current Trends in Clinical Practice. J Clin Med 2023;12:6434. [Crossref] [PubMed]
- Gao L, Goebel LKH, Orth P, et al. Subchondral drilling for articular cartilage repair: a systematic review of translational research. Dis Model Mech 2018;11:dmm034280. [Crossref] [PubMed]
- Minas T, Gomoll AH, Rosenberger R, et al. Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med 2009;37:902-8. [Crossref] [PubMed]
Cite this article as: Denwood H, Hauer TM, Berube M, Kelley MG, Cook A, Lin H, Cong T. Detriment of subchondral plate violation in antegrade osteochondral procedures—lessons and future direction. Ann Joint 2025;10:26.


